Definition:- It is a multisystem disorder of unknown etiology characterized by the development of hypertension to the extent of 140/90 mm of Hg or more with proteinuria after the 20th week in a previously normotensive or non-proteinuric woman.
PIH (Pregnancy Induced Hypertension)- This is defined as hypertension that develops as a direct result of the gravid state. It includes- GHTN, Pre-eclampsia & eclampsia.
According to ACOG-2013 Hypertensive Disorders in Pregnancy are classified as-
1. Preeclampsia and Eclampsia
2. Gestational Hypertension
3. Chronic Hypertension
4. Preeclampsia superimposed on chronic hypertension
Risk Factors:-Predisposing Factors in developing Preeclampsia are as follows –
1. Age -Extremes of age (who are first exposed to chorionic villi Young & Elderly Primigravid woman)
2. History – Family History, Previous history of Preeclampsia
3. Hyperplacentosis (When chorionic villi are growing excessively) – Multiple Pregnancy, Molar Pregnancy
4. Metabolic Disorders – Diabetes, Hyperhomocysteinemia
5. Autoimmune Disorders – Antiphospholipid antibody syndrome
6. Obesity- BMI of more than 30 kg/meters square
7. Pre Existing disorders- CKD, CVD, Thrombophilias
Etiopathogenesis:-
Basic pathology is endothelial dysfunction & intense vasospasm, affecting all the vessels particularly those of the uterus, kidney, placental bed, or brain.
(A) Hypertension:-
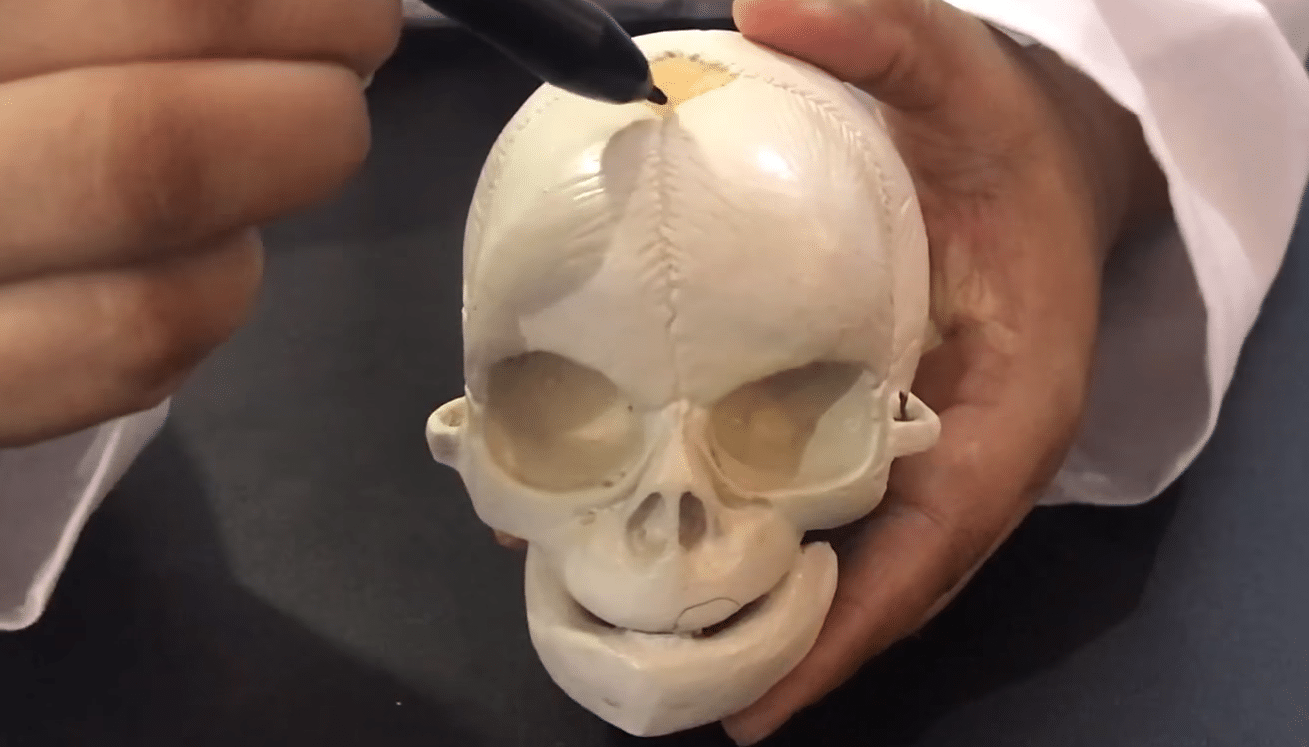
- Trophoblast invasion:-
Invasion of endovascular trophoblast into the walls of the spiral arterioles of uteroplacental bed
⇓
In 1st trimester endovascular trophoblast invades up to the decidual segment
⇓
In the second trimester, another wave of trophoblast invades up to the myometrial segment
⇓
Muscular arterial wall(endothelial lining by fibrinoid formation)
⇓
Spiral arterioles into a low resistance, low pressure, high flow system.
⇓
[in preeclampsia] there is the failure of the 2nd wave of endovascular trophoblast migration & reduction in blood supply to the fetoplacental unit.
2. Endothelial dysfunction & vasospasm:-
Endothelial dysfunction due to oxidative stress & inflammatory mediators. Vasospasm due to imbalances of vasodilators (PGI2, NO) & vasoconstrictors (Angiotension 2, TXA2 & endothelin)
- There is an imbalance in a different component of prostaglandin, deficiency of vasodilator prostaglandin(PGI2) & an increase in the synthesis of thromboxane(TXA2) a vasoconstrictor in platelet.
- Increased vascular sensitivity to the pressor agent angiotensin II, angiotensinase activity is depressed.
- Nitric oxide(NO) synthesized in the vascular endothelium relaxes smooth muscle inhibits platelet aggregation & prevents thrombosis. The deficiency of NO causes HTN.
- Endothelin-1 synthesized by endothelial cells is a vasoconstrictor, which causes HTN.
- Inflammatory mediators:- cytokines, TNF(tumor necrosis factor) interleukins(IL) derived from leucocytes causes endothelial injury.
- Abnormal lipid metabolism causes more oxidative stress by peroxides, superoxide radicals-cause endothelial injury.
(B) Edema:-
Excessive accumulation of fluid in the extracellular tissue space, due to oxidative stress causes endothelial injury leads to increased capillary permeability & leaky capillaries.
(C) Proteinuria:-
Spasm of afferent glomerular arterioles causes glomerular endotheliosis leads to increased capillary permeability & leakage of protein.
Types:–
1.Mild – Include rise of BP 140/90 mmHg but <160/110 mmHg without significant proteinuria.
2.Severe:– Persistent ≥ 160/110mmHg BP, protein excretion >5gm/24 hrs, oliguria (<400 ml/24 hrs), platelet count <100,000/mm3, HELLP syndrome, cerebral or visual disturbance, severe epigastric pain, IUGR, Retinal Haemorrhage, Pulmonary Oedema.
Clinical features:-
Frequently occurs in primigravida (70%) usually appears after 20 weeks.
- Symptoms –
Mild symptoms:–
- slight swelling over the ankles which persists on rising from the bed. The tightness of the ring on the finger, gradually swelling may extend to the face, abdominal wall, vulva, or even the whole body.
Alarming symptoms:–
- Headache – either over the occipital or frontal region
- Disturbed sleep
- Diminished urinary output <400ml/24 hr
- Epigastric pain – associated with vomiting, maybe coffee color (hemorrhagic gastritis)
- Eye symptom – blurring dimness of vision or maybe complete blindness
2. Signs –
- Abnormal weight gain ( 5 pounds a month or 1 pound in a week)
- Rise of blood pressure
- Edema over the ankles on rising from the bed.
- Abdominal examination reveals evidence of placental insufficiency or growth retardation of the fetus.
Diagnostic criteria-
- An absolute rise of blood pressure of at least 140/90 mm Hg, if previous BP is not known or rise in systolic pressure at least 30 mm Hg or rise in diastolic pressure of at least 15 mmHg over the previously known BP.
- A rise of 20 mm Hg MAP over previous reading or when MAP is 105 mm Hg or more.
- Mean Arterial pressure by Page – [ MAP ]= systolic pressure + (diastolic pressure * 2) / 3
- Edema – Pitting edema over the ankle after 12 hours bed rest or rapid gain in weight 5 lb a month or 1 lb a week.
- Proteinuria – Presence of protein in 24 hrs >3 gm or ≥ 2+ (1 gm/L) on at least 2 random clean catch urine samples tested ≥ 4 hours apart in absence of UTI is considered to be significant.
Diagnostic evaluation-
- Urine test
- Blood values (serum uric acid >4.5 mg/dl),(serum creatinine > 1 mg/dl)
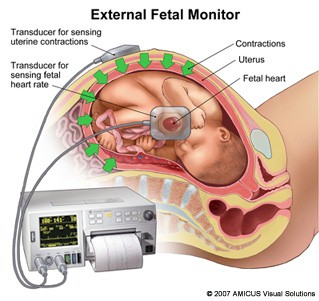
- Antenatal fetal well being monitoring – by fetal kick count, USG for fetal growth or liquor pockets, CTG, etc
- Ophthalmoscopic examination
Complication-
(a) Immediate-
1.Maternal –
During Pregnancy
- eclampsia
- Oliguria & Anuria
- Dimness of vision or Blindness
- Preterm Labour
- Cerebral hemorrhage
- HELLP syndrome (Haemolysis, elevated liver enzyme & low platelet count
- ARDS ( Acute respiratory distress syndrome)
During Labour
- eclampsia
- PPH
During puerperium
- eclampsia
- Shock
- Sepsis (operative interference)
2.Fetal –
- Intrauterine death (spasm of uteroplacental bed)
- Intrauterine growth restriction (placental insufficiency)
- Asphyxia
- Prematurity – due to spontaneous premature labor
(b) Remote-
- Residual HTN – persist even after 6 months following delivery.
- Recurrent pre-eclampsia
- Chronic renal disease
- Placental abruption
Management:-
Objectives
- To stabilize HTN & to prevent its progression to severe pre-eclampsia
- To prevent complication
- Delivery of a healthy baby in optimal time.
- Restoration of the health of the mother in the puerperium.
General management
- Ideally, all patient is to be admitted in the hospital for effective supervision. She should be warned against ominous symptoms such as headache, visual disturbance, vomiting epigastric pain, or scanty urine.
- Proper rest in bed in the left lateral position lessens the effects of vena cava compression. Also increased renal blood flow → diuresis. It also reduces blood pressure or increases placental perfusion by uterine blood flow.
- Diet with an adequate amount of daily protein (100 gm), usual salt intake is permitted, fluid need not to be restricted, total calorie approximately 1600 cal/day.
Drugs:-
1. Diuretics –
- In the case of cardiac failure, pulmonary edema, or antihypertensive drugs (where BP reduction is associated with fluid retention). Edema is not relieved by rest, use it with precaution as it causes – decreased placental perfusion & harm to the baby by an electrolyte imbalance.
- Frusemide 40 mg – 5 days/ week – PO (orally)
2. Antihypertensive –
Use while the persistent rise of BP along with proteinuria is found.
- Methyldopa – 250-500 mg TDS ( central & peripheral anti-adrenergic)
- Labetalol – 100 mg TDS ( adrenoceptor antagonist) (α or β blockers)
- Nifedipine – ( calcium channel blockers) 10-20 mg BD
- Hydralazine – 10-25 mg BD (vascular smooth muscle relaxant)
Method of delivery:-
- Induction of labor
- If aggravation of the pre-eclampsia in spite of medical treatment & appearance of epigastric pain.
- If the cervix is ripe, surgical induction by low rupture of membrane.
- If the cervix is unripe prostaglandin (PGE2) gel 500 mg intracervical in the posterior fornix is inserted after ripening, low rupture of the membrane can be performed.
- Cesarean section –When the urgent termination is indicated & the cervix is unfavorable (unripe or closed) associated with complicated factor malpresentation CPD etc.
Note – I/M ergometrine following delivery of a baby is withheld as it may cause a further rise of BP.
Download the App: Android App
For more Lectures, please visit-
YouTube Channel – NursingLecture
Facebook – Facebook Page
Check out the video of the Preeclampsia here: